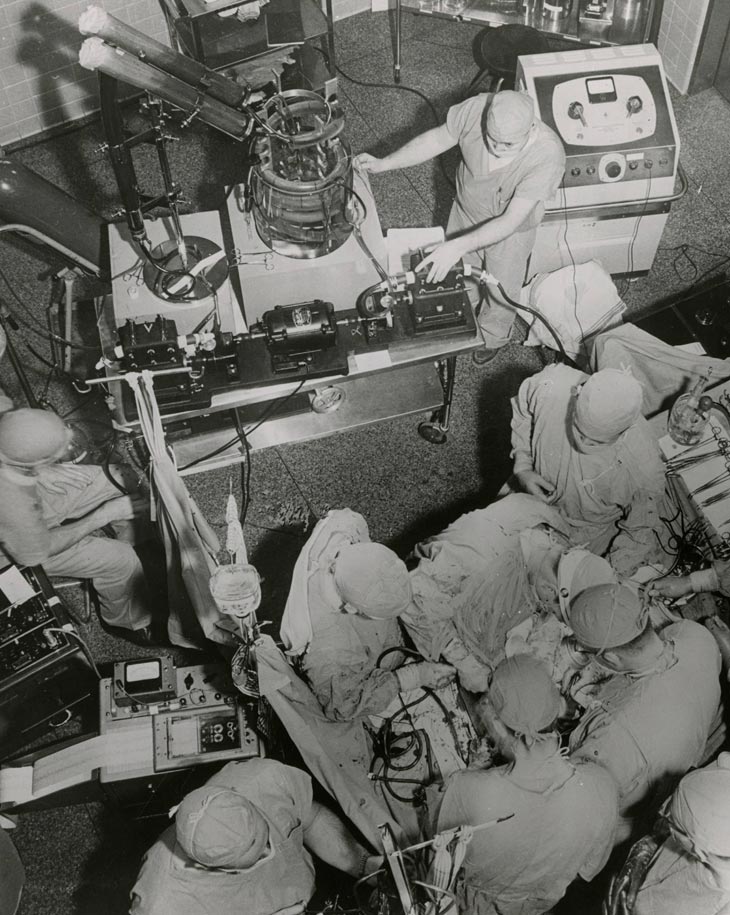
For a pump, the heart is a deceptively complex organ that has many ways to malfunction, even before birth. Until the 1940s, congenital heart disease was just accepted as an unfortunate event that was beyond medical science. In 1951, the Variety Club Heart Hospital, the first dedicated cardiac hospital in North America, was opened at the University of Minnesota. And in 1952, F. John Lewis and a team including Richard Varco, Mansur Taufic, and C. Walton Lillehei used deep hypothermia and inflow occlusion to close a 5-year-old girl’s heart defect in approximately 5 minutes. By 1955, Richard Wall and Lillehei had succeeded in designing a heart-lung machine that could oxygenate the blood during an operation, allowing the surgical field around the heart to remain dry and visible. The era of successful human open-heart surgery had been launched.
With post-operative patients at risk of heart arrhythmia, the method of attaching wires to the heart muscle to deliver an electric charge that could regulate the muscle was developed. When the hospital experienced a power failure, Lillehei turned to one of the electrical engineers, Earl Bakken (founder of Medtronic), for a solution. What resulted was the first wearable, battery-operated cardiac pacemaker in 1958.
The decades that followed saw collaborations among experts and industry that led to artificial heart valves, stents, an implantable pacemaker, and implantation of improving iterations of left ventricular assist devices (LVAD, artificial heart pump). There was groundbreaking research into the mechanics of high blood pressure, and the effects and treatment of high cholesterol.

In the past decade, Demetri Yannopoulos and Jason Bartos teamed with University engineers to redesign a different piece of lifesaving equipment, the extracorporeal membrane oxygenation machine, or ECMO. In 2015, prior to COVID-19, ECMO was not in the public eye, nor was it commonly available. Yannopoulos and his colleagues redesigned ECMO to fit in the back of an SUV—actually a small fleet of SUVs were equipped—able to deliver the equipment to patients in an emergency room of a smaller hospital. The goal is to reduce death from sudden cardiac arrest across the state, improving survival rates in smaller and more remote communities.
The quality of your healthcare should not be dependent on where you live
After a heart attack, even once circulation has been restored, some heart muscle remains “dormant” or nonfunctional. Rosemary Kelly is working to develop regenerative cellular patches to stimulate the muscle back into action and regain its pumping function.
Robert Tranquillo and his team are developing biologically-engineered vascular grafts and heart valves to repair congenital heart defects, providing a viable alternative to donor vessels and synthetic grafts, and, because they can grow with the patient, helping children avoid repeated surgeries.
Studying a beating human heart is difficult outside of the operating room. Although there are numerous 3D computational models available, a collaboration between a Disney animator and our Visible Heart Lab (and other experts) just took that simulation technology a vital step forward. Trainees can now interact with a highly accurate and detailed 3D beating heart that is fully modifiable to illustrate wall motion abnormalities and valve lesions—helping them demystify the heart a little more.
We are fortunate to have this history of innovation and innovators. It is a legacy we continue to learn from and build on every day.